Insured Americans have been ripped off for years. Fortunately, Americans in two states have new resources to protect themselves.
New state laws Tennessee (valid from July 1) and Texas (valid September 1) Now give insured Americans in individual, small business plans the ability to save money when paying cash for more affordable services while still receiving a credit discount. Tennessee extended this offer to public employees as well. These reforms break down the barriers that prevent patients from accessing the most affordable care while laying the foundation for a true market in government health care systems.
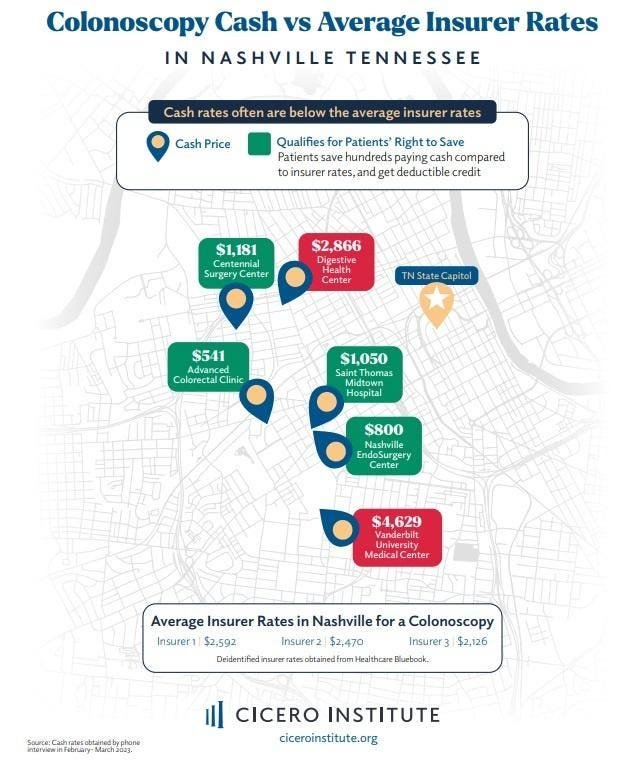
Cash prices in Nashville
We made a few phone calls recently Nashville and found we could pay $541 cash for a colonoscopy, far less than the $2,400 average rate negotiated by the three largest insurers in the state. In fact, we found at least four providers in downtown Nashville that would charge less if we paid cash instead of using our insurance card. In other words, many Americans often pay too much for services when they use their insurance. Under this new state law, people are free to access the $541 option and not be penalized by their insurer for going out of network.
Of course, it’s not the insurance companies that overpay, it’s the patients. About 94 percent of Tennessee workers have an insurance deductible, which means they pay 100 percent of most non-preventive health care costs up to their deductible. Only after that does the insurance company start paying. For many patients, a $2,400 colonoscopy comes right out of their wallets and bank accounts, leaving less money for food, mortgage payments and family expenses.
Under the new law, if a patient negotiates a lower price for a service covered by their insurance, and if the negotiated price is less than the average amount their plan pays, the patient can submit proof to their insurer. The insurer”I will calculate the full amount the covered person paid out-of-pocket to the amount of the covered person’s deductible, coinsurance, copayment, or other cost-sharing amount.” In short, a patient is free to use whichever provider offers the most affordable care, and their insurance company cannot discriminate against them for doing so.
Under the status quo, patients tend to use providers who have contracts with their insurers, often called “in-network” providers. This can mean big bills while you’re paying a deductible. The new reform allows patients to decide, with their doctors, the best care option at a price that won’t break the bank. Currently, about 40 percent of patients are bypassing they needed care because they are afraid of how many zeros will appear on the rest of their patient portal.
This new self-pay law is a step forward in empowering people with high costs chronic conditions to see who they want without potentially having to empty their wallet into insurance every year.
These new laws have been major successes, but the fight to make price transparency work for all patients will require more work. The next step is to create incentives from the rewarding insurers patients who continue to seek more affordable care postdeductible.
As more insured patients and workers are given reasons to seek affordable care, more small businesses will thrive on savings and provide benefits amid inflation.
Health professionals like these laws because they will be paid immediately, rather than spending weeks or months fighting over payments with insurance companies. And if enough patients use consumer-friendly tools to find better deals, then everyone benefits as premiums can go down next year.
Speaker Cameron Sexton (TN), Senator Shane Reeves (TN), and Representative Tom Oliverson (TX) along with others who worked on the new self-pay reform deserve a lot of credit. The push for a reform that adds this new option for patients over the objection of those who benefit from the status quo is taking a toll. Tennessee and Texas have become national leaders in price transparency, and many patients will benefit as a result.
This piece was co-written with Tanner Aliff the Policy Director for the Right to Health at the Texas Public Policy Foundation.