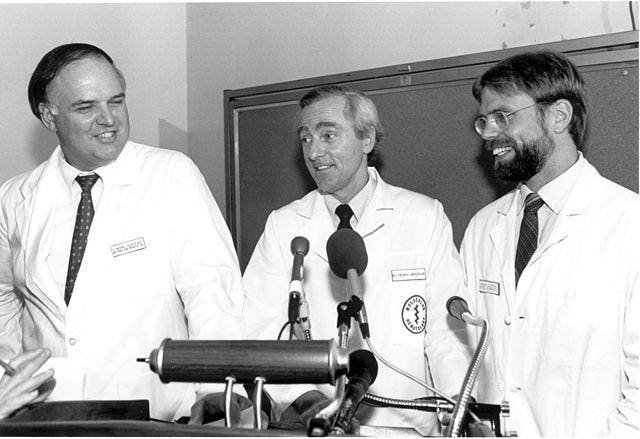
The Gene Therapy press conference held on September 13, 1990. Left to right: R. Michael Blaese, … [+]
This story is part of a series on current developments in Regenerative Medicine. In 1999, I defined regenerative medicine as the collection of interventions that restore tissues and organs damaged by disease, injured by trauma, or worn down by time to normal function. I include a full spectrum of chemical, gene, and protein-based drugs, cell-based therapies, and biomechanical interventions that achieve this goal.
In this subseries, we focus specifically on gene therapies. We explore current treatments and look at developments poised to transform healthcare. Each article in this collection delves into a different aspect of the role of gene therapy within the larger narrative of Regenerative Medicine.
The introduction of gene therapies set the stage for a dramatic change in medicine. They mark the dawn of a new era in personalized healthcare.
The 1990s were a melting pot for gene therapy, with efforts around the world pushing boundaries, driven by the bold vision of treating diseases at their root—at the genetic level. This decade saw clinical trials that provided the first definitive evidence that gene therapy was more than a science fiction myth.
Landmarks and Discoveries
In 1990, the National Institutes of Health performed one of the first gene therapy treatments. This treatment was given to two young girls. The two girls had a rare and life-threatening disorder called severe combined immunodeficiency (SCID), which was caused by a genetic mutation. SCID leads to a dysfunctional immune system, making patients vulnerable to infections and other health issues. Researchers at the NIH aimed to correct the underlying genetic cause of the girls’ SCID using gene therapy.
The treatment for SCID involved extracting blood cells from patients, genetically modifying them, and then reintroducing the modified cells into their bodies. Although not a complete cure, gene therapy had a significant positive impact on the girls’ health and quality of life. The treatment helped alleviate some of the debilitating symptoms associated with the disease, boosted their immune systems and reduced their susceptibility to infection. This discovery was a turning point in gene therapy research and demonstrated the safety and efficacy of treating genetic disorders in human patients.
Other milestone reached in gene therapy when 4-year-old Ashanthi de Silva was born the first person to be successfully treated with this technique. Ashanthi, like the previous cases, was diagnosed with severe combined immunodeficiency (SCID), a condition that severely compromises the immune system.
The treatment Ashanthi received involved inserting a functional copy of the adenosine deaminase gene into her body using a viral vector. Viral vectors are genetically engineered viruses that deliver therapeutic genes to target cells. This gene therapy treatment used adeno-associated virus (AAV) as the viral vector.
In Ashanthi’s case, the viral vector carried a functional copy of the adenosine deaminase gene into her body. This allowed her body to produce the missing enzyme, restoring her immune system’s ability to fight infection.
A fatal setback for gene therapy
Despite the positive progress of gene therapy, a tragic setback happened when 18-year-old Jesse Gelsinger died during a gene therapy trial for metabolic liver disease, shaking the field and prompting a reevaluation of safety protocols.
In 1999, Gelsinger, who had a genetic liver disease called ornithine transcarbamylase deficiency, participated in a gene therapy trial at the University of Pennsylvania. The trial aimed to develop a treatment for infants with severe forms of the disease. Despite having a milder form of the disorder, Gelsinger volunteered for the trial and was given an injection of an adenoviral vector carrying a corrected gene.
Unfortunately, she suffered from a severe immune reaction to the viral vector used in the gene therapy. This immune response triggered a series of events that led to multiple organ failure, ultimately resulting in his untimely death just four days after receiving the injection.
The adverse immune reaction Gelsinger experienced highlights a critical challenge in gene therapy research. In his case, the immune response to the adenoviral vector caused an overwhelming inflammatory response in his body, leading to systemic complications and organ dysfunction. This severe reaction underscored the importance of careful evaluation and mitigation of potential risks associated with viral vectors used in gene therapy.
However, we push forward
The ramifications of Jesse Gelsinger’s death were significant. That was the result a lawsuit, a government investigation, the suspension of gene therapy trials in the United States for a period and the implementation of new regulatory procedures for gene therapy trials. Gene therapy was still relatively new and uncharted territory. This lack of precedent and experience led to a trial-and-error approach that often faced ethical concerns.
Despite the challenges, the 1990s was a decade of innovation and success stories that laid the foundations for modern gene therapies. A major breakthrough in the previous trials was the delivery of genes into the body using genetically modified viruses called viral vectors that target specific cells for therapeutic gene delivery. Retroviruses and adeno-associated viruses were developed as vectors for efficient and safe gene delivery.
Key tools and innovations for gene therapies
Despite the challenges, the 1990s was a decade of innovation and success stories that laid the foundations for modern gene therapies. An important breakthrough in the previous trials was the delivery of genes into the body using genetically modified viruses called viral vectors that target specific cells for therapeutic gene delivery. Retroviruses and adeno-associated viruses were developed as vectors for efficient and safe gene delivery.
Retroviruses, for example, integrate their genetic material into the host cell’s DNA, allowing the therapeutic gene to become a permanent part of the cell’s genome. Adeno-associated viruses, on the other hand, can exist in an episomal form within the cell, providing a more transient but efficient means of gene transfer. These viral vectors are designed to facilitate targeted gene transfer without causing harm to the host.
A Legacy of the Past & The Promise of the Future
The gene therapies that have emerged in recent decades represent human ingenuity and perseverance. The 1990s was a defining period, marking the transition from theoretical position to real-world application. Understanding the context and history of gene therapy during this period is crucial assessing the present situation of art and preparation for the future.
By revisiting this critical era in the development of gene therapy, stakeholders, researchers, and enthusiasts alike can gain an updated perspective on the field, its progress, and milestones yet to be achieved. The legacy of gene therapy in the 1990s will be the treatments developed and the lessons learned, shaping the ethical and regulatory fabric that will support the gene therapies of tomorrow.
As we move forward, guided by the legacy of the past and the promise of the future, gene therapy remains a beacon of hope for the countless individuals who may one day benefit from its groundbreaking applications.
To learn more about regenerative medicine, read more stories at www.williamhaseltine.com
1 Comment
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?